Project ECHO prepares doctors to manage addiction care closer to home
By Katherine Brind’Amour
For patients suffering from opioid use disorder, and for the physicians in small towns across Pennsylvania who are their first level of care, Project ECHO offers hope. The effort aims to give primary care physicians the tools they need to treat the growing group of Pennsylvanians addicted to opioids—many of whom live in regions with no specialized addiction resources. It’s a win-win: patients get a doctor who can treat them close to home, and physicians get to expand their knowledge, their professional network and their relationship with their patients.
The concept comes from a physician at the University of New Mexico who wanted to shorten the wait list at his gastroenterology clinic. Now, more than 220 institutions around the world use Project ECHO for at least 90 disease topics. And Penn State Health researchers hope to influence them all.
“Research evaluating the project hasn’t kept pace with growth of the movement clinically,” says Dr. Jennifer Kraschnewski, director of Project ECHO at Penn State College of Medicine and a Penn State Health primary care clinician-investigator who studies community health interventions. “It is our goal to create an evidence base to support the model and its ability to mentor primary care providers outside of urban academic hubs. We also aim to learn how to best grow and use Project ECHO as an intervention.”
Penn State expert clinicians are halfway through their first cohort of the Opioid Use Disorder Project ECHO, funded by a grant from the Substance Abuse and Mental Health Services Administration.
“What most excites me is that Project ECHO gets to the heart of the challenges of treating some of a physician’s toughest patients,” says Dr. Sarah Kawasaki, director of the Opioid Use Disorder Project ECHO at the College of Medicine. She is also director of Addiction Services for Pennsylvania Psychiatric Institute. “We’re creating a community to support and educate physicians and improve the chances that they can provide the care their patients need, rather than sending them to a specialist for first-line treatment.”
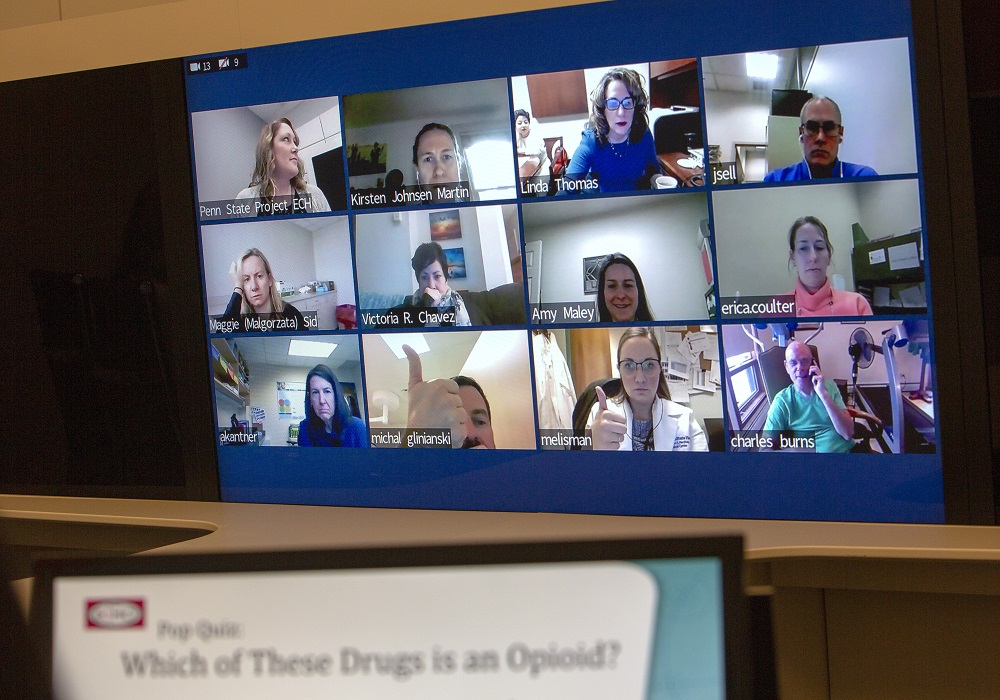
The program series includes 12 sessions, each of which is attended by up to 20 clinicians plus Kawasaki and her Project ECHO team. The Penn State team is comprised of other addiction experts from the College of Medicine and partner organizations. It serves as the hub, with each participating clinic a spoke learner. At each session, they discuss a complex patient case that has been deidentified and sent in by a participating clinician. They then listen to a short lecture. The project rolls from one group to the next, growing a network of specially trained physicians. In time, it should exponentially build the state’s ability to bring best-practice care to all patients.
Two attendees from The Wright Center for Community Health, a state-designated Center of Excellence in addiction and recovery, were part of the first Project ECHO group in November. Like Kawasaki’s program, The Wright Center is one of the state’s eight hubs for the Pennsylvania Coordinated Medication-Assisted Treatment (PAC-MAT) program. Another two physicians in the first group are from spokes of The Wright Center’s PAC-MAT program.

Primary care providers discuss a patient case and the latest research on addiction.
“Providing care in the addiction and recovery space for less than three years, we have an insatiable desire to learn and develop courses to support our physician-led care teams,” says Dr. Linda Thomas-Hemak, chief executive officer of The Wright Center. “That is why we signed up for ECHO.” Thomas-Hemak is also board-certified in internal medicine, pediatrics and addiction medicine.
“The physician who shares a challenging case gets peer and expert guidance to directly help that one patient,” says Thomas-Hemak. “But the project’s reach is much broader. It affects care of the total population as we have similar cases come up. And we’re just the first group—there will be a force-multiplying impact of engaging the provider workforce in this learning network. That’s really powerful.”
Thomas-Hemak views the project’s unmeasured effects on physician culture as a game changer. She believes it helps lower physicians’ fear of dealing with a subject that was often not taught in medical school.
“Project ECHO takes the education outside of Penn State and puts it into the state of Pennsylvania,” Kawasaki says. “It reduces physician burn-out by giving them the tools and support they need to be effective. It broadens the reach of addiction-related knowledge and fights the opioid problem in a meaningful way.”
Efforts at Penn State currently include the opioid use group and a BSA (formerly Boy Scouts of America) project to help summer camps in the region talk about ways to improve healthy eating options. Because ECHO is part of the Penn State Clinical and Translational Science Institute, Kraschnewski expects the program will cover many other clinical fields in the future, and she already has autism on the list to tackle.
The continued success of Project ECHO depends on grant money, though. The team has applied for a $100 million grant. If they succeed, the grant would support Project ECHO in 15 counties for three years.
“We need to get specialty knowledge out to the places where it doesn’t currently exist,” says Kraschnewski, who is also vice chair of clinical research for the Department of Medicine at Penn State Health Milton S. Hershey Medical Center. “Our goal is to educate the clinic spokes so that more communities have physicians who can treat opioid use disorder, just like they have for diabetes or high blood pressure.”
About CTSI
Penn State Clinical and Translational Science Institute provides the tools, resources and training to help the Penn State community move its health research out of the science laboratories and into use by the people and communities who need it. Through its cores, the institute provides research tools, advanced biostatistical expertise, funding programs for exploration of unique research ideas and a dedicated team for partnering with the community more effectively in research. In addition, the institute trains the next generation of researchers.

Dr. Sarah Kawasaki leads Penn State’s first Project ECHO cohort.
If you're having trouble accessing this content, or would like it in another format, please email the Penn State College of Medicine web department.
